Updated on June 24, 2025
Epilepsy is a neurological condition characterized by recurring seizures, episodes of abnormal electrical activity in the brain, sometimes referred to as "electrical storms" inside the brain. These episodes can cause temporary changes in movement, consciousness, behavior, and emotions.
Epilepsy affects people of all ages and can develop for many reasons—brain injuries, infections, genetics, developmental disorders. However, many cases do not have an identifiable cause.
While there is no cure for epilepsy, it can be managed with treatment, and many people with epilepsy are able to lead full, active lives.
How is epilepsy treated?
The main goal of treating epilepsy is to prevent seizures—ideally, and if possible, eliminating seizures entirely. The primary treatment for epilepsy is medication. Special diets, medical devices, and in some cases, surgery, are also used in treatment. Minimizing treatment side effects and improving a person's quality of life are other important treatment goals.
Treatment recommendations will vary from person to person and will depend on multiple factors, including the type of seizures a person is experiencing, how frequently seizures occur, a person's age, their overall health, and how they respond to treatment. Coexisting and underlying medical conditions are another important consideration, especially if these are in some way related to seizures.
People respond differently to different therapies, and finding the right therapy or combination of therapies can take time.
Treatment options for epilepsy
- Anti-seizure medications (previously known as anticonvulsants or antiepileptic drugs). These drugs work by stabilizing electrical activity in the brain. There are many different types of anti-seizure medications, which work through different mechanisms.
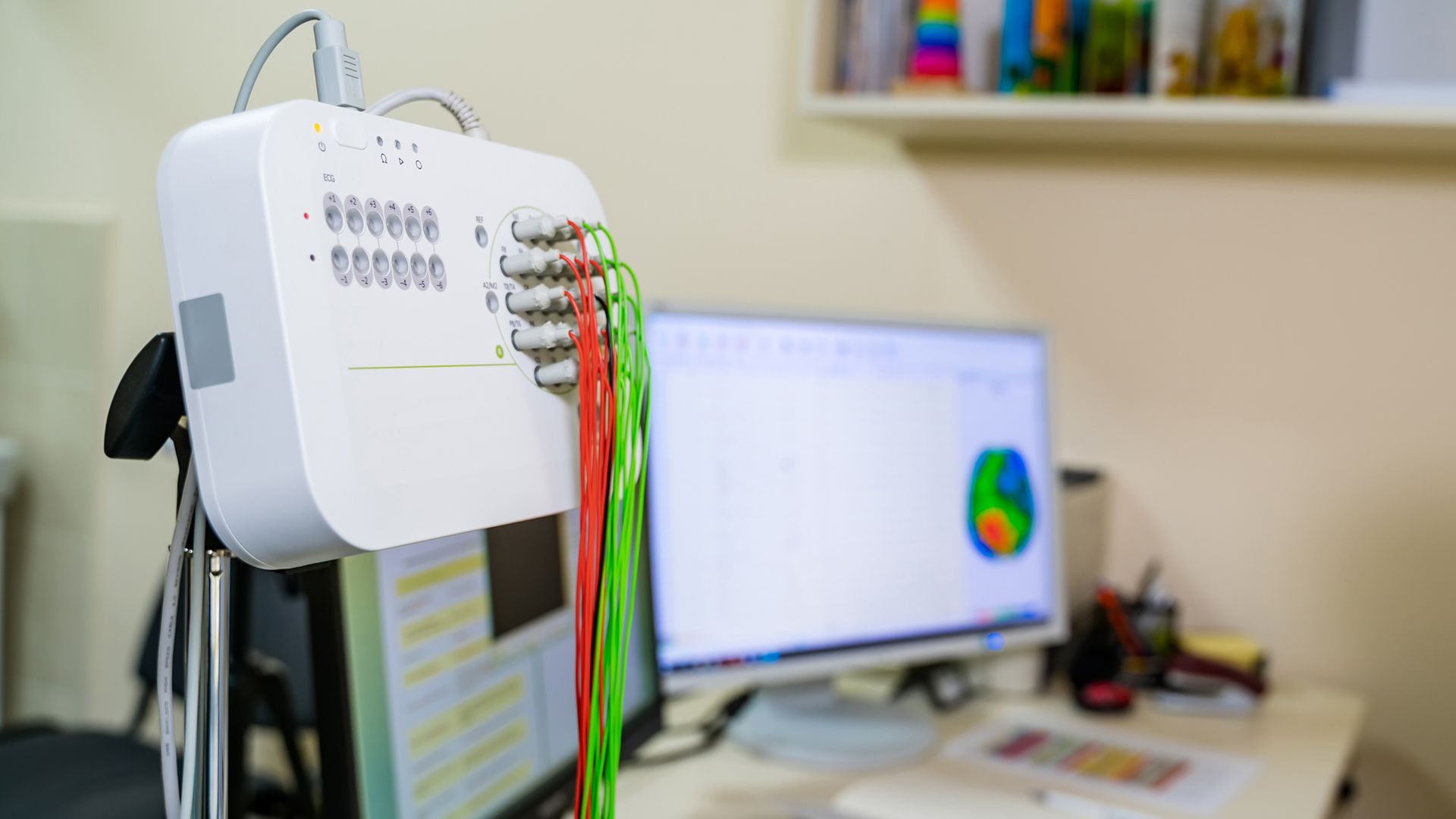
- Other treatment options may be considered if seizure control cannot be achieved with medications. These can include specialized diets (like the ketogenic diet), implantable devices (such as vagus nerve stimulation), or surgical procedures to remove the area of the brain where seizures originate.
- Lifestyle modifications can also play an important role in treatment. This can include steps to maintain a regular sleep schedule, steps to reduce or manage stress, and avoiding known seizure triggers.
In addition to treating seizures, counseling and social support can be important parts of a treatment plan, and this can make an important difference in the lives of people and families affected by epilepsy.
Questions when starting a new treatment
Mentioned above, finding the right therapy or combination of therapies can take time. A person's treatment plan may also change for other reasons, such as changing treatment needs or new medications becoming available.
Here are some questions to ask your healthcare team if you or a loved one are discussing a new therapy for epilepsy:
When discussing a new medication:
- What is the name of the medication and the dosage?
- How does this medication work to prevent seizures?
- How is the medication administered and how often?
- What is the goal of this medication? How will we know if it is working?
- What are the potential side effects? Is there a risk of serious side effects?
- How will a person feel while taking this medication?
- Are there things a person will need to avoid while taking this medication? For example, certain foods, activities, or other medications?
- Is this medication safe to use during pregnancy?
- Can this medication interact with other drugs or supplements? Always tell your healthcare provider about all medications you are taking, including medications for other conditions, over-the-counter medications, and supplements.
- Can this medication lower the effectiveness of birth control?
- What will this medication cost? Who can I talk to if I have concerns about the cost of this medication?
- What should a person do if they miss a dose?
- Are there any limitations on activities? For example, sports, driving, heights, or swimming.
When discussing surgery or a medical device:
- What is the name of the procedure or device?
- What is the goal of this treatment? What kind of seizure control can we expect?
- What are the potential risks or side effects?
- Does the person being treated need any tests or evaluations before this treatment?
- What healthcare provider will perform this procedure?
- What will this treatment cost?
- What will the recovery process be like?
- How will this affect everyday life and activities? Are there any restrictions on activities?
When discussing dietary treatment:
- What is this diet called? Why is it being recommended?
- How does this diet help with seizure control?
- What foods will the person need to avoid? What will they need to include in their diet?
- Are there risks or side effects associated with this diet?
- Will I be working with a registered dietitian?
- How will we know if this diet is working?
Remember, if you have questions, need an explanation, or have concerns, your healthcare providers will always be your best source of information. Managing epilepsy is a collaborative process, and good communication between you and your healthcare team is essential to getting the best care possible for yourself or your loved one.