Updated on May 10, 2023.
The potential side effects that some people might temporarily experience after a COVID-19 vaccination have been well documented: soreness or pain at the injection site, fatigue, a slight fever, chills, nausea, body aches, headache.
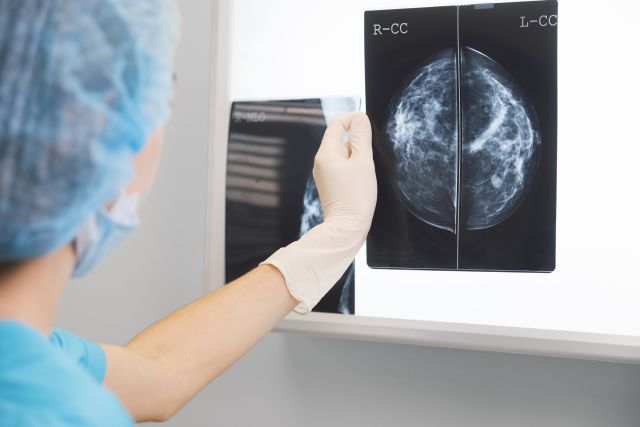
There is no link between COVID-19 vaccines and breast cancer, but a lesser-known effect is swollen lymph nodes in the armpit area—and they could raise a false alarm when they appear on some imaging tests, particularly routine mammograms.
Swollen lymph nodes after a COVID vaccination aren’t typically a cause for concern. In fact, the harmless swelling is a normal response in many people. It’s a sign that your lymph nodes are doing their job and stimulating your immune system to protect you from the coronavirus that causes the disease.
Why do lymph nodes swell?
Lymph nodes contain white blood cells that fight infection. Underarms contain a cluster of about 20 to 40 lymph nodes. When the immune system detects the presence of a potentially harmful substance, such as bacteria, viruses, chemicals or pollen, it increases white blood cell production. This can also happen with some vaccines.
The white blood cells attack the foreign substance, leading to swollen lymph nodes. You might even feel a tender lump or swelling in your armpit. The lump or swelling should go away within a few days or weeks. (But if it doesn’t, let your healthcare provider know.)
When lymph nodes under the arms appear larger than normal on a screening exam like a mammogram, they can sometimes indicate the presence of breast cancer or other cancers like lymphoma and leukemia. Unfortunately, radiologists can’t discern the cause of swollen lymph nodes under the arms (called axillary lymphadenopathy) that appear on your mammogram, so additional imaging tests are usually needed.
For many recently vaccinated women who have no other breast cancer symptoms, this could result in unnecessary testing and anxiety.
That’s why the Society of Breast Imaging advises women to schedule their screening mammograms before their first COVID-19 vaccine or wait four to six weeks after their last dose to schedule their exam. By then, the swelling should subside.
This delay can help you avoid an abnormal mammogram result because of your vaccination. The recommendation applies only to women with no symptoms who are scheduling their routine annual screening.
A noticeable trend seen on mammograms
Lisa A. Mullen, MD, an assistant professor of radiology in the Breast Imaging Division of Johns Hopkins University School of Medicine, first noticed an uptick of swollen underarm lymph nodes among healthcare workers undergoing annual breast screenings shortly after their COVID vaccine. She and other breast imagers began comparing notes. They realized the rise in larger than normal nodes might not be a coincidence.
They surmised that the increase in swollen lymph nodes was related to the newly introduced Pfizer and Moderna vaccines. Since healthcare workers were among the first groups eligible to receive those vaccines, the association between swelling and the immunizations made sense.
“The Pfizer and Moderna vaccines are causing a pretty significant immune response, and that’s why we’re seeing those lymph nodes in the underarm,” Dr. Mullen explains. Both vaccines are messenger RNA vaccines—commonly called mRNA vaccines. mRNA vaccines are a new type of vaccine that works differently than other vaccine types, such as those for the flu, to trigger an immune response.
The swelling tends to appear in the same arm as the vaccine injection. Radiologists have also seen enlarged lymph nodes in the area above the collarbone. Mullen points out they’ve appeared in computed tomography (CT) scans of the neck, chest and heart in addition to breast imaging, including MRI mammograms and ultrasounds.
Similar observations have been cited by radiologists at Massachusetts General Hospital and Weill Cornell at New York-Presbyterian in a January 19 article published in Clinical Imaging and a February 5 article published in the American Journal of Roentgenology.
Swollen lymph nodes in vaccine clinical trials
In clinical trials, 11.6 percent of people ages 18 to 64 who received the Moderna vaccine experienced swollen or tender lymph nodes after their first dose, the Centers for Disease Control and Prevention (CDC) reports. The second dose yielded a 16 percent rate of swelling.
Among those 65 and older, 6.1 percent and 8.4 percent had swollen lymph nodes after their first and second dose, respectively.
In the Pfizer clinical trials, the percentage of recipients who had abnormal lymph nodes was lower than in the Moderna trials. It’s too soon to know whether the reaction is limited to mRNA vaccines. Such reporting isn’t available for the single-dose Johnson & Johnson shot, which is a viral vector vaccine that works differently than the Moderna and Pfizer mRNA vaccines.
Follow-up exams for swollen lymph nodes
What happens if you undergo a mammogram shortly after your vaccination and you have swollen lymph nodes? You’ll likely be called back for further evaluation, Mullen said, usually with an underarm ultrasound to look more closely at the lymph nodes and measure their size.
You’ll then need to return sometime after your ultrasound to see whether your lymph nodes have calmed down. “For a totally healthy asymptomatic woman,” Mullen adds, “we’re recommending a follow-up in three months.”
Recalls can be anxiety-producing for patients, Mullen says. “Patients are worried that we’re seeing a breast cancer. But all we’re seeing is a big lymph node because of their vaccine. But we’re obligated to treat it as if it could be a sign of breast cancer.”
One way to help prevent anxiety and additional testing is to follow the Society of Breast Imaging recommendations to wait four to six weeks for a screening after vaccination.
That said, you should never delay a diagnostic mammogram, which, unlike a screening mammogram, is intended to evaluate the cause of symptoms common to breast cancer.
“If a patient has any symptoms at all that she’s worried about that relate to her breast or underarms, such as a breast lump, breast pain or nipple discharge, she should talk to her healthcare provider (HCP), Mullen advises. “She should not delay any type of evaluation. It could be that it’s COVID vaccine-related. But if we don’t know, it’s not good to assume and we don’t want the [Society of Breast Imaging] recommendations to delay necessary patient care.”
You also shouldn’t delay your COVID shot if you’re set to be vaccinated shortly before a breast cancer screening that you can’t reschedule. Before you’re screened, tell your healthcare provider and mammogram technologist that you were recently immunized against COVID and in which arm the vaccine was injected. If the radiologist sees swelling, it coud help with the interpretation of your results, and you might be able to avoid unnecessary follow-up testing.
Get screened as soon as it’s safe
Try not to put off a screening mammogram longer than necessary. If you skipped your annual mammogram last year because of the pandemic, it’s important to schedule one as soon as possible.
Most organizations like the American Cancer Society and the U.S. Preventive Services Task Force publish guidelines that advise women with an average breast cancer risk to start annual screenings at age 40 to 50.
The recommendations are as follows:
American Cancer Society (ACS): Women can start screening between ages 40 and 45 if they so choose. Beginning at 45, the ACS recommends annual mammograms. From 55 to 74, getting screened every one or two years is recommended.
American College of Obstetricians and Gynecologists (ACOG): Starting at age 40 until at least age 75, average-risk women should be offered the option. By 50, all women should be screened every one or two years.
National Comprehensive Cancer Network (NCCN): Yearly mammograms should start at 40.
United States Preventive Services Task Force (USPSTF): Between 40 and 74, women should have mammograms every other year.
Talk with your HCP to determine the best screening schedule for you.