7 key questions to ask your gynecologist
If you've ever wondered these things, you're not alone. Here's how to prepare for your next OBGYN appointment.
Updated on July 10, 2024

Unpredictable periods, vaginal changes, how to avoid sexually transmitted infections—you’re not the only one wondering about health issues like these.
Allison Giles, DO, an OBGYN in Richmond, Virginia, shares the questions she gets asked most often, plus the answers everyone should know. Of course, if you’re experiencing new or worsening symptoms your OGBYN should know about, make an appointment right away to get some answers.
Can you get tested for every cancer?
There are three main gynecological cancers, says Dr. Giles: ovarian, uterine, and cervical. You can be screened for cervical cancers, but for the other two, a healthcare provider (HCP) will determine how to test based on your symptoms.
Ovarian cancer: There’s no reliable screening test for ovarian cancer, which is often caught in later stages. But HCPs can sometimes use an ultrasound to look for tumors on your ovaries or a CA-125 blood test to check levels of the protein CA-125. This protein can be elevated in people with ovarian cancer. Neither of these tests are completely accurate, which is why it’s so important to tell an HCP as soon as you notice any ovarian cancer symptoms, such as fullness or discomfort in the lower abdomen, irregular vaginal bleeding, or fatigue most of the time.
Uterine cancer: There’s no screening test, but your OBGYN will check for suspicious symptoms during routine exams. “If you have bleeding after menopause, for example, we’ll perform an endometrial biopsy to test for uterine cancer,” Giles says. “That involves taking samples of uterine tissue to see if it contains abnormal or cancerous cells.”
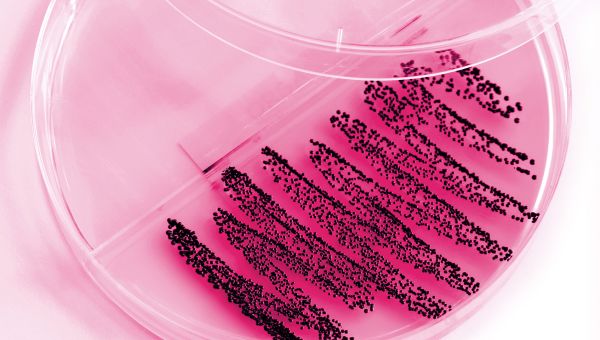
Cervical cancer: A Pap test screening for cervical cancer is used to detect two things. “One is the presence of abnormal cervical cells; the other is the human papilloma virus (HPV), which causes cervical cell changes,” says Giles. “If you’re at low risk for cervical cancer, you don’t need an annual Pap. Women ages 21 to 30 at low risk should have one every three years—and you don’t need to get the HPV test during Pap tests until age 30.” Between ages 30 and 65, you should have a Pap test alone every three years, an HPV test alone every three years, or a combination Pap and HPV test every five years.
Talk to your OBGYN or another HCP about your recommended screening schedule, as well as additional exams that may be included in regular checkups.

Are my periods 'normal?'
“There’s a wide variety of ‘normal’ periods,” says Giles. “A lot of people think theirs are too heavy or too light, when really, they’re fine. A typical menstrual cycle can be anywhere from 21 to 35 days long, and a period may last anywhere from 1 to 7 days. Blood flow is usually heavier at the beginning and then lighter towards the end. But even that’s not true for everybody.”
How can you help your HCP determine if your period is typical? Track it. Simply write down the day it begins each month, or Giles recommends using a period tracker app, such as Pink Pad. “These apps help me get a snapshot of what's happening with your menstrual cycle. Instead of trying to piece together a pattern based on memory, they let me see exactly what you’ve experienced over recent months,” she says.
In addition to tracking how long and heavy your periods are, take note of any symptoms you have. Tell your HCP if they’re severe or interfere with your daily activities. Conditions such as premenstrual dysphoric disorder and endometriosis are sometimes dismissed as PMS or heavy periods.

Are periods even necessary?
“Another question I get asked is, ‘Are periods medically necessary?’” says Giles. “And the answer is no, they’re not. Some people like to see them every month to know they're not pregnant. Others are happy to let their periods go. Both options are safe.”
There are several birth control methods that can help to either lighten your periods or get rid of them altogether for as long as you’re on the medication. Options include the continuous use of birth control pills, progestin injections (Depo-Provera), birth control implants, intrauterine devices (IUDs), and vaginal contraceptive rings.
Ovulating less over the course of your reproductive years could help lower ovarian cancer risk. Hormonal birth control methods that prevent or reduce ovulation may offer some protection.

What’s the best birth control?
“People want to know: Is this the best birth control for me? And I won't have an answer unless you come in and chat with me,” says Giles. “Then, we can figure out your specific needs. But, in general, we’ve seen a surge in people interested in long-acting, reversible contraceptives, such as IUDs, and implantable devices like Nexplanon.”
Reversible devices are extremely safe, effective, and can be removed when you’re ready to start a family, she explains. “Nexplanon is a tiny rod we place in your arm, which can last for three years. An IUD is a small device that’s placed in the uterus. IUDs come in two varieties: ones with hormones, and ones without,” she continues. “The hormone-free one, ParaGard, is made of copper and can last up to 10 years. IUDs with hormones include Mirena, Skyla, Kyleena, and Liletta. These all have a form of the hormone progesterone, which makes uterine lining thin, so periods are lighter.”
There are also pills that offer different hormone levels. You and your HCP need to make an individual decision about which pill might be best for you.
“And then there’s the vaginal ring, which is a flexible device you place in your vagina,” Giles says. “You leave it in for three weeks, take it out, get a period, and then put a new one in. It’s a nice middle ground between remembering the pill every day and long-acting reversible contraceptives.”

How do you deal with vaginal dryness?
During menopause, many people notice vaginal irritation and dryness due to decreasing estrogen levels, says Giles. “There are many different options, including lubricants, medications, and noninvasive procedures to help cope with this.”
“Lubrication is a must at this age, both for pleasure purposes and also safety,” she adds. “Dry vaginal tissue is more prone to injury during intercourse, so it's important to maintain lubrication.”
People who are post-menopausal and have vaginal dryness may benefit from local estrogen, available in creams, tablets, and vaginal rings. “Topical estrogen is safe for the majority of people because it’s not absorbed into the bloodstream as much as the oral formulations can be. It stays in the area it's applied—in this case, the vagina—and helps to increase the health and the blood flow to those tissues,” says Giles.
There are also nonhormonal over-the-counter vaginal moisturizers and lubricants. Moisturizers are applied every two or three days, while lube can be used whenever you have sex.

Can you cure my STI?
“Sexually transmitted infections (STIs) are common, and a lot of people want to know, is this the type that’s with you forever or is it the type that can be cured with antibiotics?” says Giles. “The STIs that can be treated with antibiotics and cleared up completely are gonorrhea, chlamydia, and trichomoniasis. Syphilis is also treatable with antibiotics. The ones that will stay with you for life are herpes and HIV,” she adds. About 5 percent of people who are infected with hepatitis B will go on to have chronic issues, as well.
Hepatitis C, which is transmitted by blood-to-blood contact, has traditionally been an illness that stays with you for life. It’s now considered curable with new (and expensive) medications.

Can oral sex spread STIs?
“People often wonder if oral sex is really a way to transmit diseases. And certainly, the answer is yes,” says Giles. Herpes, chlamydia, syphilis, and HPV can be transmitted via oral sex, among many other infections.
“HPV can cause cervix changes, as we mentioned before, but when spread through oral sex, it can result in throat cancer as well,” she explains. “There’s a vaccine to help protect against the cancer-causing strains of HPV, so all young boys and girls should get the full series of shots from their pediatrician.”
Children should receive the two-dose HPV vaccine between the ages of 11 and 12, although it may be given as early as age 9. If a teenager hasn’t gotten the vaccine yet, they should get it as soon as possible. After age 14, three shots are needed instead of two. People who have not previously been vaccinated can receive the vaccine until age 26, but being vaccinated at older ages is less effective for lowering cancer risk. In some circumstances, an HCP may recommend the vaccine up until age 45.
Always ask new male partners or those with unknown STI statuses to wear a condom during oral sex; female partners should wear dental dams. Find out about free, fast, and confidential STI testing near you.

American Cancer Society. Can Ovarian Cancer Be Found Early? Page revised on July 24, 2020. Accessed June 2022.
Centers for Disease Control and Prevention. Sexually Transmitted Diseases. Page reviewed January 13, 2022.
Mayo Clinic. Estrogen (Vaginal Route). May 1, 2022. Accessed June 2022.
Mayo Clinic. CA 125 test. March 31, 2022. Accessed June 2022.
Centers for Disease Control and Prevention. Uterine Cancer: What Should I Know About Screening? August 5, 2021. Accessed June 2022.
American Cancer Society. Can Ovarian Cancer Be Prevented? April 18, 2018. Accessed June 2022.
Mayo Clinic. Vaginal dryness after menopause: How to treat it? June 18, 2022. Accessed June 2022.
Centers for Disease Control and Prevention. Hepatitis C (pdf). April 2020. Accessed June 2022.
Centers for Disease Control and Prevention. Sexually Transmitted Diseases (STDs): STD Risk and Oral Sex—CDC Fact Sheet. December 31, 2021. Accessed June 2022.
American College of Obstetricians and Gynecologists. Long-Acting Reversible Contraception (LARC): Intrauterine Device (IUD) and Implants. November 2021. Accessed June 2022.
American College of Obstetricians and Gynecologists. The Menopause Years. November 2021. Accessed June 2022.
Centers for Disease Control and Prevention. Viral Hepatitis: Hepatitis B Questions and Answers for Health Professionals. March 30, 2022. Accessed June 2022.
Centers for Disease Control and Prevention. Vaccines and Preventable Diseases: HPV Vaccination Recommendations. November 16, 2021. Accessed June 2022.
Mayo Clinic. Delaying your period with hormonal birth control. Page revised January 8, 2022. Accessed June 2022.
Mayo Clinic. Menstrual Cycle: What’s normal, what’s not? Page revised April 29, 2021. Accessed June 2022.
Office on Women’s Health. Birth control methods. Page revised November 24, 2021.
U.S. Preventive Services Task Force. Cervical Cancer: Screening. Page revised August 21, 2018. Accessed June 2022.
National Cancer Institute. Cervical Cancer Screening (PDQ)—Patient Version. June 10, 2022. Accessed June 2022.
More On


video

article

slideshow


video


video
