Which birth control option is right for you?
From pills to patches, get the lowdown on your options for contraception.
Updated on April 25, 2024

When it comes to birth control, there are more options than ever before. But with so many to choose from, it’s hard to know which route is right for you.
Some methods contain hormones that work by interfering with ovulation, or the release of the egg from the ovaries. Some disrupt the fertilization process, which is the meeting of the sperm and egg. Others hamper the implantation process, which is the attachment of an embryo (the dividing cells made from the egg and sperm) to the uterine wall. Other devices simply block the sperm from reaching the egg.
When you're choosing birth control, it’s important to remember that you’ll want to protect yourself from sexually transmitted infections (STIs), too, and not all methods do.
If you’re on the hunt for a contraceptive, the best thing to do is to talk to your healthcare provider (HCP) about the possibilities and pros and cons of each, and how each type fits with your overall health profile. In the meantime, here’s a guide to help you keep your options straight.
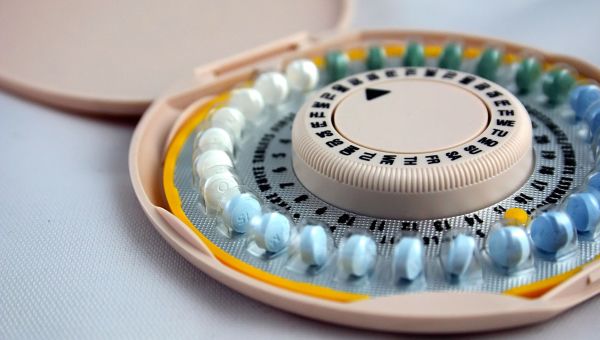
Hormonal Methods
Traditional hormonal birth control methods are popular and come in a variety of forms, including pills, rings, and patches.
These methods contain either progestin only (the synthetic form of progesterone) or a combination of estrogen and progestin. The progestin-only option works by thickening cervical mucus to make it difficult for sperm to fertilize an egg. Hormone combination methods work by preventing ovulation altogether.
According to the American College of Obstetricians and Gynecologists (ACOG), just 9 percent of women taking combined hormonal birth control will become pregnant during the first year after starting these methods. (This is with typical use of the products, accounting for some missed pills and occasional misuse.) When used correctly 100 percent of the time, fewer than 1 out of every 100 women will become pregnant within the first year of use. Progestin-only methods have similar success rates.

Forms of Hormonal Birth Control
Hormonal birth control comes in the following forms:
Pills: Some combination pills are taken continuously for 21 days then stopped or replaced with placebo pills for the following 7 days. Others are taken continuously for 86 days followed by a 7-day course of placebo pills. Other options are taken non-stop for 365 days straight to prevent or reduce bleeding altogether. Progestin-only pills (or “minipills”) are taken continuously for 28 days without any placebo pills.
Rings: Vaginal rings contain estrogen and progestin. They're inserted into the vagina, where they stay for 21 days, and are then removed for 7 days, at which time you’ll get your period. You'll likely need a new ring each month, though rings that can be reused for 13 cycles are available.
Patches: Patches that contain both estrogen and progestin are placed on the skin of the buttocks, chest (anywhere except the breasts), upper back, arms, or abdomen so that the hormones can be absorbed through the skin into the body. The patch should be changed out every week for three weeks. On the fourth week, you remove the patch and get your period.
Implants: Inserted into the upper arm, this matchstick-size rod contains progestin and lasts for about three years.
Injections: Progestin-only shots are given every 13 weeks by an HCP, and the first one can be given any time during your cycle (as long as you’re not pregnant).
Some of these hormonal methods can be taken or used continually without skipping a week, so talk with your HCP about the best choice for you.
Note that it may take some time after you stop taking hormonal birth control to get pregnant if you choose to do so. Most people can get pregnant a few months after they stop birth control, but the time may vary depending on your health profile. Ask your HCP about what you can expect.

Is Hormonal Birth Control Right for You?
There are some people who may be advised not to take combined estrogen-progestin oral contraceptives. These may include people who:
- Are 35 years or older who smoke 15 or more cigarettes per day
- Have multiple risk factors for heart disease (including smoking, diabetes, and high blood pressure)
- Have high blood pressure, with readings of 160 mm Hg or more systolic or 100 mm Hg or more diastolic
- Have venous thromboembolism (a blood clot that starts in a vein) and are not taking an anti-clotting medication
- Have known coronary artery disease
- Have a history of stroke
- Have breast cancer
- Have had diabetes for more than 20 years or who have diabetes with complications such as kidney disease or eye or nerve issues related to diabetes
If you have any of these conditions, or any other chronic conditions, make sure to check with your HCP before starting any hormonal birth control.

IUDs
Many experts recommend intrauterine contraceptive devices (IUDs), a form of long-acting reversible contraception (LARC). IUDs are small, T-shaped pieces of plastic that are inserted into the uterus and left in for up to 3 to 10 years at a time, depending on the type.
Some hormonal IUDs release progestin, which helps to thicken cervical mucus, making it harder for the sperm to reach the egg in the fallopian tubes. Progestin also causes the lining of the uterus to thin, which makes it difficult for implantation to occur. Copper IUDs release copper, which restrict sperm’s mobility, and in turn, make it harder for sperm to reach the egg.
According to ACOG, IUDs are 20 times more effective than hormonal methods like pills, patches, or rings. While the hormonal IUD can help decrease bleeding, the copper IUD is more likely to increase bleeding. Work with your HCP to determine if a hormonal or nonhormonal option is best for you.

Barrier Methods
Barrier methods block sperm from getting to the egg. There are a variety of types; some can be purchased over the counter while others require a prescription. Many people opt for these contraceptives because they're hormone-free and easily accessible. About 18 to 28 women out of 100 will become pregnant when using these techniques for a year. Barrier methods include:
- Diaphragm: Before sex, a reusable cup made of latex or silicone is placed deep into the vagina, covering the cervix. A diaphragm is used with spermicide and must be left in place for 6 hours after sex but removed within 24 hours.
- Cervical cap: Similar to a diaphragm, a cervical cap is a small plastic dome that’s placed over the cervix. It’s also used with spermicide and must stay in place for 6 hours after sex, but no longer than 48 hours total.
- Condom: A male condoms is made of rubber, plastic, latex, or animal casings. It’s placed over the penis and worn during sex. A female condom is a thin plastic pouch that slides inside the vagina and is held in place by rings at both ends. Condoms help prevent pregnancy and sexually transmitted infections (STIs), although male condoms are slightly more effective against STIs than female condoms. Important to note: Both types of condoms should not be used together. Water-based or silicone lubricants are safe to use with condoms. Just be careful not to use lubricant made with oil, as it can damage latex condoms and cause them to break.
- Spermicide: Spermicides come in a variety of forms, including gels, foams, creams, or suppositories, all of which contain a chemical called nonoxynol-9, which destroys sperm. The spermicide is inserted into the vagina, close to the cervix. It takes 10 to 15 minutes before it’s effective, and that effectiveness wears off an hour after application.
- Sponge: Filled with spermicide, this round, disposable foam device is inserted into the vagina to cover the cervix. The sponge can be inserted up to 24 hours before sex and should stay in place for 6 hours after, but should not be worn for longer than 30 hours.

Natural Methods
Natural birth control methods can usually be followed without a prescription or specific device. The withdrawal method, or coitus interruptus, involves pulling the penis out of the vagina right before ejaculation, or the release of semen. It’s still possible for sperm to enter the vagina, however, if there is some pre-ejaculation fluid containing sperm or if the penis isn’t fully withdrawn before ejaculation begins. According to ACOG, up to 22 women out of 100 may get pregnant using the withdrawal method as birth control over the course of one year.
Lactation amenorrhea (LAM) is based on breastfeeding. For women who have recently given birth, nursing exclusively prevents ovulation, which makes it impossible to get pregnant. There are some guidelines, though: Breastfeeding must be done every four hours or more during the day, and every six hours or more during the night. What’s more, this method should only be used for up to six months after birth, or until a woman’s period returns. Although research in the United States is sparse on the topic of LAM, Planned Parenthood reports that just 2 out of 100 women using LAM correctly would get pregnant in the six months post-birth.
Of course, completely abstaining from all sexual activities, including vaginal and anal sex, is considered to be 100 percent effective in preventing pregnancy. Even during anal sex, there is a chance that semen can make its way into the vagina.

Fertility Awareness Methods
In a nutshell, fertility awareness means knowing when you’re the most fertile and using that to either boost or lower your chances of becoming pregnant. There are a variety of ways to do so, including the standard days method, basal body temperature (BBT) method, and cervical mucus method.
The standard days method takes into account the length of your typical menstrual cycle to calculate your most fertile days. Many women with a cycle lasting between 26 and 32 days are most fertile between days 8 and 19. For those who wish to prevent pregnancy, abstaining from sex (or using other forms of contraception) during that time is key.
The basal body temperature (BBT) method involves taking your temperature at the same time every morning before you get up and move about. During ovulation (when you’re most fertile), your temperature usually rises 0.5 to 1 degree, and then stays higher through the end of your cycle. Women are most fertile on the two to three days prior to the temperature increase. There are several smartphone apps that can help track your BBT and inform you whether it’s “safe” to have sex.
The cervical mucus method simply involves observing your cervical mucus. During your most fertile days, or the days around ovulation, you should notice thin, slippery mucus similar to the consistency of egg whites. To prevent pregnancy, avoid intercourse or use a barrier method whenever you have slippery mucus.
When used correctly 100 percent of the time to prevent pregnancy, 1 to 5 women out of 100 will get pregnant when using a fertility awareness method for a year. With typical use, 12 to 24 women out of 100 will become pregnant during that one-year timeframe.

Sterilization
Sterilization procedures are for those who want permanent birth control, and there are options for both men and women.
For successful fertilization to occur, an egg released from the ovaries must travel through the fallopian tubes to find the sperm. A procedure called tubal ligation—also known as having your tubes tied—closes off the fallopian tubes so this cannot happen. Tubal ligation can be done as an outpatient procedure anytime or following a vaginal birth or C-section. The technique is very effective: Fewer than 1 out of 100 women will get pregnant within a year.
A man can have a vasectomy to lower the chances of a woman becoming pregnant. During this procedure, the vas deferens—a tube which carries sperm from the testes—is cut, tied, clipped, or sealed so the sperm cannot be released and therefore cannot meet the egg. In terms of preventing fertilization, a vasectomy is only slightly less effective than tubal ligation.
Sterilization is meant to be permanent. In some cases, these procedures can be reversed, but it may be difficult to get pregnant afterwards.

Emergency Contraception
It’s possible that some birth control methods will break, become dislodged, or fail during intercourse. If this happens, you may want to consider emergency contraception options, which can lower the chances of pregnancy after the fact.
Copper IUDs are the most effective for emergency contraception, as they make it difficult for the sperm to fertilize the egg. They must be inserted within 5 days after unprotected sex by an HCP, and after that, they can be used for long-term birth control for up to 12 years. When copper IUDs are inserted within those 5 days, it’s predicted that they can prevent more than 99.9 percent of pregnancies. Some hormonal IUDs can also be used for emergency contraception.
Emergency contraception pills are another form of emergency contraception that should be used as soon as possible after sex in order to be effective. Otherwise known as the morning-after pill, there are two types available in the U.S. They prevent or slow ovulation or lower the chances of fertilization. These options include:
- A pill that contains levonorgestrel, a type of the female hormone progestin. This is available in several brands that can be purchased over the counter.
- A pill that contains ulipristal acetate, a progestin receptor modulator. This option must be prescribed by an HCP.
These types of “morning-after” pills are most effective when used within 72 hours after intercourse. Ulipristal acetate is the more effective option overall, especially if taken after that 72-hour window and up to five days afterwards.
When deciding on birth control, talk with your HCP. Together, you can decide on the most effective option for you.

The American College of Obstetricians and Gynecologists. Combined Hormonal Birth Control: Pill, Patch, and Ring. Last reviewed March 2018.
The American College of Obstetricians and Gynecologists. Progestin-Only Hormonal Birth Control: Pill and Injection. Last reviewed October 2020.
The American College of Obstetricians and Gynecologists. Long-Active Reversible Contraception (LARC): Intrauterine Device (IUD) and Implant. Last reviewed May 2020.
The American College of Obstetricians and Gynecologists. Barrier Methods of Birth Control: Spermicide, Condom, Sponge, Diaphragm, and Cervical Cap. Last reviewed February 2018.
Centers for Disease Control and Prevention. Coitus Interruptus (Withdrawal). Last reviewed February 1, 2017.
The American College of Obstetricians and Gynecologists. Postpartum Birth Control. Last reviewed May 2020.
Planned Parenthood. Breastfeeding. Page accessed November 18, 2021.
Office of Population Affairs. Contraception and Preventing Pregnancy. Page accessed November 18, 2021.
The American College of Obstetricians and Gynecologists. Effectiveness of Birth Control Methods. Copyright October 2021.
The American College of Obstetricians and Gynecologists. Fertility Awareness-Based Methods of Family Planning. Last reviewed January 2019.
The American College of Obstetricians and Gynecologists. Sterilization for Women and Men. Last reviewed March 2019.
The American College of Obstetricians and Gynecologists. Emergency Contraception. Last reviewed June 2020.
Planned Parenthood. How effective are IUDs? Page accessed November 18, 2021.
Planned Parenthood. How does the copper IUD work as emergency contraception? Page accessed November 18, 2021.
Planned Parenthood. Which kind of emergency contraception should I use? Page accessed November 18, 2021.
More On


video

article


video


video
