Updated on April 1, 2022.
Stable angina is a condition where you develop episodes of chest pain or other heart symptoms in response to exertion or strain. The condition is caused by blockages or narrowing in the heart’s arteries.
The symptoms of stable angina last about 5 minutes or less each wave, and they go away with rest or medicine. Stable angina episodes are predictable and one episode is pretty much like another.
What’s not so clear-cut is how best to treat stable angina.
While many heart doctors have long thought that a minimally invasive procedure to open up a blocked artery or arteries is beneficial, a landmark 2017 study shook up the field by suggesting that careful treatment with medication might work as well in some cases. The study raised many questions, and heart doctors continue to discuss it today, along with other research that has emerged since then.
Here’s what you should know about stable angina and how it’s treated.
What causes stable angina?
Usually, stable angina happens when you have plaque buildup in one or more of the blood vessels that supply blood to your heart muscle. These blood vessels are called coronary arteries, and they narrow down when you have coronary heart disease, which is related to risk factors like unhealthy cholesterol levels, diabetes, and smoking.
With normal physical activity, like walking from one room to another, enough blood typically gets through that narrowed artery so that you feel fine.
But when you put more strain on your heart—such as by walking upstairs—the artery is too narrowed by the plaque to deliver the extra blood your heart needs. That imbalance, called myocardial ischemia, causes the symptoms of stable angina. These may feel like chest pain or pressure, fullness, or squeezing, and may occur in the neck, shoulder, jaw, arm, or back. Nausea, vomiting, or shortness of breath may also occur, especially in women. (In addition to exertion, stable angina can also result from emotional distress, hot or cold weather, heavy meals, or smoking.)
If you think these sound like heart-attack symptoms, you’re right. Angina and heart attacks both start with ischemia, but with angina, the lack of blood supply is reversible. Heart attack, where a clot inside the vessel breaks off, clogs it, and causes part of the heart muscle to die, is a serious complication of myocardial ischemia.
Another type of angina can arise if very tiny blood vessels in your heart, but not the main coronary arteries, narrow down. It is treated with medications and lifestyle changes, including exercise. A third type of angina is caused by the blood vessels spasming.
What happens after a diagnosis?
If your healthcare provider (HCP) suspects you have stable angina—also known as chronic coronary syndrome—they will want to check the overall health of your heart, including how many blood vessels are affected by coronary disease. Tests may include:
- Blood tests
- An electrocardiogram (ECG), which records the electrical activity of the heart
- A stress test, such as on a treadmill
- A CT scan, a type of detailed X-ray
- Coronary angiography, in which a catheter is threaded up toward your heart and dye is released to show the contours of the arteries
- A heart ultrasound, also called an echocardiogram, to look at how strongly your heart squeezes
With this information, you and your HCP are in a better position to talk about treatment.
How is stable angina treated?
One approach is with medications. Your HCP may give you nitroglycerin to take during the episodes of pain. This is a drug that causes arteries to widen temporarily and the heart’s blood supply to increase. Other options include:
- Medications for high blood pressure
- Anti-clotting drugs
- Cholesterol-lowering drugs
It’s also important to treat other conditions that could be contributing to the angina, such as:
- High blood pressure
- Fast irregular heartbeat, such as atrial fibrillation
- Thyroid problems
- Anemia
- Heart valve problems
Another treatment approach for stable angina is called revascularization, which means physically opening up the blocked artery or arteries. There are two ways to do this. One way is with open-heart surgery, called coronary artery bypass grafting.
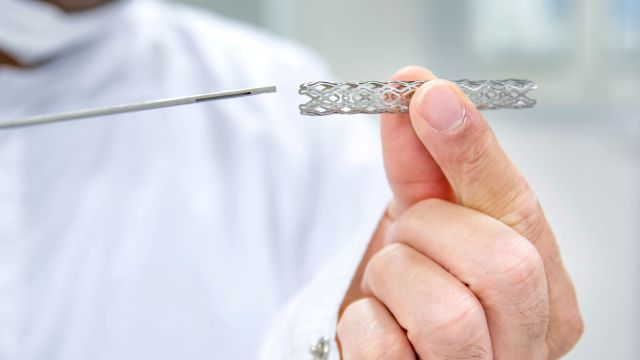
The other way is with a procedure called percutaneous coronary intervention, or PCI. Also called coronary angioplasty with stenting, this minimally invasive procedure lets a cardiologist put a stent—a tiny mesh tube just a tad wider than a toothpick—into a blocked or narrowed artery.
What is the ORBITA trial and what did it show?
Studies show that stenting saves lives during heart attacks, and it has long been a common way to manage stable angina, too. Based on suggestions from some studies and the experience of many cardiologists, it seemed to stand to reason that opening blockages in this way would help angina patients find relief.
But direct, rigorous, scientific evidence had been lacking. So, a group of heart researchers did a study called ORBITA (short for Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina) that compared stenting plus medication to medication alone for people with angina.
The study, published in 2017 in The Lancet, included 200 patients with stable angina and severe blockage in a single coronary artery. About half underwent coronary angioplasty with stenting. For the other half, the control group, the procedure was stopped at the point where a stent would be inserted.
Neither the patients nor the researchers knew who received a stent. (The fact that there was a control group is unusual in a study of this kind, but very important for the sake of comparison and the placebo effect.) In addition to both groups undergoing the procedure, both groups were also carefully treated with medication. The only difference was whether they actually got a stent.
After six weeks, both groups were evaluated for chest pain frequency and again given a treadmill exercise test. The researchers had been confident that stenting plus medication would win out, but the results were a surprise. The findings suggested that the two approaches were about the same in terms of helping people with stable angina tolerate exercise. Patients who received the stent did not have significantly greater improvement in exercise time or reduction in chest pain frequency.
Lyndon Box, MD, an interventional cardiologist at West Valley Medical Center in Caldwell, Idaho, praises the way the study was conducted. But, he says, there are important factors to consider in evaluating the results:
- It was a small study. According to Dr. Box, cardiology studies usually involve 1,000 or more patients. A larger study may or may not have shown benefit.
- Study participants had a blockage in only one artery. “Most people who need stents have more than one blocked,” he says. “Only about 1 in 10 people with a single blockage get a stent.”
- It’s a short study. “The follow up was pretty short, only six weeks, so you don’t know how these people are going to do a year or two later,” Box says.
Overall, Box says, “I’m probably in the camp of people that don’t actually see this making a big difference.” His concern is that studies like this “can often get overinterpreted as simply thumbs up, thumbs down, stents are good, stents are bad.”
More recently, a study of over 5,000 patients called ISCHEMIA (International Study of Comparative Health Effectiveness With Medical and Invasive Approaches) compared PCI with medical therapy in people who had stable angina and moderate ischemia. The study found that, over a period of about 3 years, the procedures added to medicines didn’t reduce heart attacks or deaths compared to just medicines. But the procedures did do a better job of improving symptoms. The results were published in Circulation in 2020 and 2021.
But ORBITA and ISCHEMIA were different. For one thing, ORBITA looked at exercise tolerance and ISCHEMIA looked at heart attack rates. For another, the types of patients each study chose to focus on had some differences. Comparing these studies, therefore, is like comparing apples to oranges, a common situation in medical science, and many questions still remain. Scientists are planning a follow-up called ORBITA-2.
Is a stent right for you?
For heart attacks, stenting is beneficial. “For people who have heart attacks, or what we call acute coronary syndrome, there’s definite, overwhelming data that doing an intervention, or stenting, reduces the risk of death, repeat heart attacks, heart failure, and dangerous arrhythmias,” says Box.
For people with stable angina, though, the benefit of stenting over and above careful treatment with medication isn’t as clear.
As with all medical procedures, there are risks to stenting, so it’s important to discuss those with your HCP, along with the goals of the procedure. Fortunately, according to Box, you have time to learn what you need to know.
“One of the good things about stable heart disease is that it’s not an emergency like a heart attack,” he says. “If you’re unsure about the procedure, it’s okay to stop and think about it, get a second opinion.”
If you have stable angina and your cardiologist recommends a stent, be sure to understand the risks and benefits given your unique situation. Ask questions and talk about your options. A frank discussion can help both you and your HCP determine if a stent is right for you.