Leukemia
- What is leukemia?
- How common is leukemia?
- What are the types of leukemia?
- What are the signs and symptoms of leukemia?
- What causes leukemia?
- What are the risk factors for leukemia?
- How is leukemia diagnosed?
- What are the stages of leukemia?
- How is leukemia treated?
- What are the possible complications of leukemia?
- When should you see a healthcare provider?
- Can you prevent leukemia?
- What is the outlook for people with leukemia?
- Living with leukemia
- Featured leukemia articles
Introduction
Leukemia is an umbrella term for certain cancers of the blood and the body’s blood-forming tissues. It’s the most common type of cancer among children younger than 15, although most cases occur in adults older than 55. Symptoms of leukemia can include fatigue, fever, swollen lymph nodes, and frequent infections. Leukemia is treatable, but a timely diagnosis is key to achieving a positive outcome for many with the condition.
Get the facts about leukemia, including its types, symptoms, risk factors, and what treatment options are available for this blood cancer.
What is leukemia?

Leukemia is a cancer that develops in bone marrow, the spongy tissue in the center of most bones that creates blood cells. Bone marrow is a part of the body’s lymphatic system, the network of tissues, organs, and vessels that helps your body absorb fats and maintain healthy fluid levels. The lymphatic system is also a component of the immune system, which serves to protect your body from potentially harmful agents like viruses and bacteria.
Bone marrow is responsible for producing multiple types of blood cells. These include:
- Platelets: Cells that help blood form clots
- Red blood cells (RBCs): Cells that transport oxygen from the lungs to the body, then carry carbon dioxide back to the lungs to be exhaled
- White blood cells (WBCs): Cells that help fight off infections and diseases
Leukemia tends to begin in immature WBCs called stem cells, although RBCs and platelets may also be involved. The cancer typically occurs in granulocytes or lymphocytes. These are types of white blood cells that travel throughout the body to protect against potential threats like viruses. Leukemias that develop from granulocytes are called myeloid leukemias, while leukemias that grow from lymphocytes are known as lymphocytic leukemias.
How does leukemia form?
Leukemia doesn’t form solid tumors like many other cancers do. It begins when abnormal changes (mutations) begin in a developing white blood cell, which causes it to multiply uncontrollably or fail to die off as usual. The abnormal WBCs—called leukemia cells—eventually crowd out other cells in the bone marrow, resulting in fewer healthy blood cells being produced and released into the body.
How common is leukemia?
Leukemia is the eleventh most common cancer in the United States, accounting for 3 percent of all new cancer cases, according to the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results (SEER) program. The NCI also states:
- Around 1.6 percent of people will be diagnosed with leukemia at some point in their lives.
- The rate of new leukemia cases is 14 per 100,000 people each year, according to data collected between 2016 and 2020.
- An estimated 59,610 cases of leukemia will be diagnosed in the U.S. in 2023.
While most cases occur in adults over age 55, leukemia is the most common cancer diagnosed in children and teens aged 15 and younger. It comprises nearly one in three childhood cancers, according to the American Cancer Society (ACS). The International Agency for Research on Cancer (IARC) reports that leukemia was the 13th most common cancer worldwide in 2020, comprising 2.6 percent of all cancers (excluding nonmelanoma skin cancer).
What are the types of leukemia?
Leukemia is classified as myeloid (or myelogenous) or lymphocytic based on the type of white blood cell from which it originates. It’s also labeled as acute or chronic according to how rapidly the cancer grows. Acute leukemia progresses quickly and features immature WBCs, while chronic leukemia tends to develop slowly and involves more mature WBCs.
Based on these characteristics, leukemia is generally divided into four main types:
Acute lymphocytic leukemia (ALL)
Acute lymphocytic leukemia is the most common type of leukemia. Also called acute lymphoblastic leukemia, ALL typically occurs in children, accounting for three out of four leukemias diagnosed in kids and teens. This type of leukemia most often develops between the ages of two and five, although older children and adults can also experience ALL.
ALL is an aggressive cancer that begins in the bone marrow’s lymphoid cells (from which lymphocytes develop). It usually spreads (metastasizes) to other areas of the body, often through blood in various organs, including:
- Lymph nodes. Also called lymph glands, these pea-sized organs are found throughout the body, including the neck, armpits, groin, chest, and abdomen. As the primary organs of the lymphatic system, they help filter and remove waste substances from the body.
- Liver
- Spleen
- Brain
- Spinal cord
- Testicles (in people assigned male at birth)
Once viewed as an incurable disease, ALL now has multiple effective treatment options. Between 30 to 40 percent of adults and nearly 80 percent of children with ALL are cured.
Chronic lymphocytic leukemia (CLL)
Chronic lymphocytic leukemia develops in lymphoid cells in the bone marrow. It’s the most common type of chronic (slowly growing) leukemia, though it rarely affects children. More than three-quarters of CLL cases occur in adults older than 60, with the average age of diagnosis being around 70 years old.
It’s possible to live with CLL for several years and feel fine. In around 2 to 10 percent of cases, CLL undergoes what’s known as “Richter’s transformation” and evolves into lymphoma, another type of blood cancer that mainly affects lymph tissues.
Over time, cancer cells can grow and spread to other areas of the body, including the lymph nodes, liver, and spleen. Some people who are diagnosed with CLL may not receive treatment right away, either because they have yet to develop signs and symptoms that require treatment or due to the risk of complications associated with getting treatment too early. Having CLL is believed to increase a person’s risk of other cancers, likely due to changes in the immune system.
Acute myeloid leukemia (AML)
Acute myeloid leukemia is the most common type of rapidly growing leukemia in adults, although it can occur in people of any age. It starts in immature granulocytes that divide uncontrollably in the bone marrow.
Like ALL, AML is an aggressive cancer that can quickly reach other areas of the body, including the:
- Lymph nodes
- Liver
- Spleen
- Brain
- Spinal cord
- Testicles (in people assigned male at birth)
An early diagnosis and intensive therapy are key to achieving a positive outcome with AML. With treatment, around 20 to 40 percent of people survive for at least five years without the cancer returning. Cancer recurrence is common in AML, especially within the first five years after treatment.
One notable subtype of AML is acute promyelocytic leukemia. It occurs when promyelocytes—a type of immature white blood cell—build up in the bone marrow and drive out healthy blood cells. Acute promyelocytic leukemia is often diagnosed around age 40, and more than 90 percent of people with this cancer achieve long-term survival.
Chronic myeloid leukemia (CML)
Chronic myeloid leukemia originates in the bone marrow’s granulocytes, though some leukemia cells may start in the liver or spleen. It typically affects adults between the ages of 40 and 60. CML is also the most common type of chronic leukemia in children—occurring more often in teenagers than young kids—although this cancer is still rare in young people.
CML may not cause symptoms for several weeks, months, or years after it develops. This type of leukemia was once associated with poor outcomes, but advances in CML treatments now help around 90 percent of people with this cancer type survive at least five years (and in many cases, at least 10 years) after treatment.
Uncommon types of leukemia
Other, less common types of leukemia and related blood disorders include:
- Hairy cell leukemia: This type of leukemia occurs when the bone marrow produces too many lymphocytes, which become abnormal and resemble small hairs under a microscope.
- Adult T-cell leukemia: Also referred to as T-cell lymphoma, or ATLL, adult T-cell leukemia is an aggressive, rapidly spreading cancer that can be found in multiple areas of the body, including blood, lymph tissues, and skin.
- Myelodysplastic syndrome (MDS): This refers to a group of conditions that are generally recognized as precancerous. It occurs when blood-forming cells in the bone marrow become abnormal and hinder healthy blood cell production. MDS eventually turns into acute myeloid leukemia in around 10 to 30 percent of cases.
- Myeloproliferative disorders: Also referred to as myeloproliferative neoplasms, myeloproliferative disorders are a group of conditions in which the bone marrow creates too many or too few platelets, red blood cells, or white blood cells. Chronic myeloid leukemia is sometimes considered a type of myeloproliferative disorder. In some cases, these disorders evolve into acute leukemia.
What are the signs and symptoms of leukemia?
Leukemia symptoms can vary based on the type and stage of the cancer. In general, some of the more common signs and symptoms of leukemia include:
- Lingering fatigue
- Weakness
- Fever or chills
- Unusually pale skin (in people with light skin tones) or grayish skin (in people with darker skin tones)
- Easy bruising or bleeding
- Swollen, tender lymph nodes
- Heavy sweating, particularly at night
- Unexplained weight loss
- Frequent, recurring infections
- Petechiae (small red, purple, or brown dots underneath the skin)
- An enlarged spleen or liver
- Frequent nosebleeds
- Bone pain or tenderness
- Joint pain
- Shortness of breath
- Rapid heart rate or chest pain
Many people with chronic leukemias don’t experience any noticeable symptoms in the cancer’s early stages. The early symptoms of acute leukemias are often vague (for example, fatigue, fever, and night sweats) and are typically attributed to more common causes such as a cold or the flu.
If leukemia spreads to other parts of the body, signs and symptoms may involve:
- Changes in vision, hearing, facial muscles, or balance (if leukemia cells travel to the brain), along with headaches, stroke and vomiting.
- A sensation of abdominal fullness (if leukemia cells cause spleen or liver enlargement)
- Small, discolored masses (leukemia cutis) that can form on the gums, eyes, or on or under the skin
What causes leukemia?
Cancer is caused by abnormal changes (mutations) to the DNA of cells. DNA (deoxyribonucleic acid) is genetic information that essentially tells a cell how to function, grow, and die in a healthy way. Leukemia occurs when a cell in the bone marrow mutates and begins to multiply uncontrollably or fails to die at the end of its standard life span. Eventually, abnormal cells collect in the bone marrow and crowd out healthy cells.
The exact mechanisms that cause leukemia aren’t always clear. Research shows that certain risk factors— like exposure to toxins or hereditary conditions such as Fanconi anemia or Down syndrome—can increase a person’s chances of developing leukemia. A virus known as human T lymphotropic virus 1 (HTLV-1) is linked to adult T-cell leukemia, although this is rare.
Leukemia has also been tied to the Epstein-Barr virus, a type of herpes virus known for causing infectious mononucleosis (mono, commonly called the “kissing disease”). It’s also been linked to many other diseases, including Hodgkin’s lymphoma and non-Hodgkin’s lymphoma, multiple sclerosis (MS), and Graves’ disease—an autoimmune disease that causes the immune system to mistakenly attack healthy tissue in the thyroid gland, leading to thyroid disorders such as hyperthyroidism.
What are the risk factors for leukemia?
Leukemia can affect anyone, though certain factors may increase your risk of developing the condition. Established risk factors for leukemia include:
- Smoking: There are dozens of cancer-causing substances in cigarette smoke. Research suggests around 20 percent of acute myelogenous leukemia cases are linked to smoking.
- Exposure to chemicals: Prolonged exposure to high levels of certain chemicals, including benzene, is associated with an increased risk of leukemia. Benzene is found in gasoline and some detergents, plastics, and pesticides. Research is ongoing to investigate the role that formaldehyde may play as a risk factor for leukemia. Formaldehyde is used in some building materials, cleaning products, and soaps. Exposure to Agent Orange—a chemical used extensively during the Vietnam War to destroy vegetation—is also connected to an increased risk of chronic lymphocytic leukemia.
- Inherited conditions: Some uncommon genetic conditions are known to slightly increase a person’s chances of developing leukemia. These include Down syndrome, Fanconi anemia, Bloom syndrome and ataxia-telangiectasia.
- Family history: Having a first-degree blood relative (such as a sibling or parent) with chronic lymphocytic leukemia may mean you’re at higher risk of developing the condition. Still, the majority of people with leukemia don’t have a close family member with the condition.
- Previous cancer treatment: Receiving radiation therapy or chemotherapy for a previous cancer can increase a person’s risk for leukemia in the future, as these treatments may trigger abnormal changes in cellular DNA.
It’s important to remember that having one or more leukemia risk factors doesn’t mean you’re sure to develop the condition, and many people with leukemia don’t have any known risk factors.
How is leukemia diagnosed?
To rule out or diagnose leukemia, a healthcare provider (HCP) will typically employ a number of different tests and scans. These may include the following:
Physical exam for leukemia
An HCP will likely begin with a physical exam to check for signs of blood cancer. These might include swollen lymph nodes, skin rashes, pale or grayish skin, or swelling that could indicate an enlarged liver or spleen. Your HCP will also ask you questions about your symptoms, medications or supplements you’re taking, and your personal and family medical histories.
Blood testing for leukemia
Blood testing is a key part of diagnosing leukemia. Based on your physical exam, your HCP may order one or more of the following blood tests:
- Complete blood count (CBC): A CBC test measures levels of platelets, red blood cells, and white blood cells. If you have leukemia, your white blood cell count will likely be elevated.
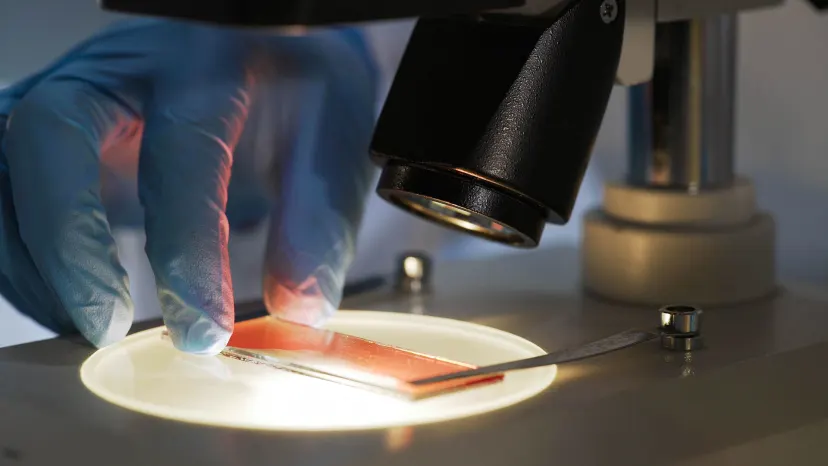
- Blood smear: During a blood smear test, a small sample of blood is examined under a microscope to check for abnormal-looking cells.
- Flow cytometry: A flow cytometry test is used to identify what types of cells are in the blood and bone marrow, as well as the amount of DNA in those cells.
Bone marrow biopsy for leukemia
Your HCP will also likely recommend a bone marrow biopsy if a blood test shows abnormal results. During this biopsy (also known as a bone marrow aspiration), a long, thin needle is inserted into the hip bone to draw out a sample of bone marrow. This sample is viewed under a microscope to check for leukemia cells.
Additional tests and scans for leukemia
If your HCP confirms a leukemia diagnosis, additional tests may be recommended to see if leukemia cells have traveled to other parts of the body. For instance, a spinal tap may be performed to test for leukemia cells in the fluid that surrounds the spinal cord and brain.
Imaging methods like X-ray, computed tomography (CT), ultrasonography, and magnetic resonance imaging (MRI) can show if leukemia has affected surrounding organs and tissues. Tests such as immunohistochemistry and molecular genetic studies will also likely be performed to learn more about your cancer’s specific type and genetic traits.
What are the stages of leukemia?
Staging is used to describe the extent of a person’s cancer. Many cancers that form tumors are staged according to the widely used TNM (tumor, node, metastasis) system, but blood cancers like leukemia are different. Each type of leukemia has its own classification system to summarize the amount of leukemia in a person’s body and whether distant organs or tissues are affected.
Acute lymphocytic leukemia stages
Acute lymphocytic leukemia (ALL) doesn’t have a standard staging system. Instead, HCPs use terms to describe how ALL is responding to treatment. These include:
- ALL in remission: There are no signs of ALL following treatment.
- Minimal residual disease: Testing shows some ALL cells in the bone marrow, but the cancer appears to be in remission.
- Refractory ALL: ALL is not improving with treatment.
- Relapsed (recurrent) ALL: ALL has returned after treatment.
- Untreated ALL: ALL has recently been diagnosed and has not been treated.
Chronic lymphocytic leukemia stages
Chronic lymphocytic leukemia is typically staged according to the Rai system in the U.S., which involves five stages:
- Stage 0: Lymphocytosis (elevated levels of lymphocytes in the blood) is present, but there are no other physical symptoms of leukemia.
- Stage 1: Lymphocytosis and swollen lymph nodes are present, but there is no spleen enlargement, anemia, or low platelet count.
- Stage 2: Lymphocytosis is present and the liver or spleen are enlarged, sometimes along with the lymph nodes.
- Stage 3: Lymphocytosis and anemia are present, sometimes with swollen lymph nodes and an enlarged liver or spleen.
- Stage 4: Lymphocytosis is present, platelet levels are low, and the lymph nodes, spleen, or liver may be enlarged. Anemia may also be present.
Acute myeloid leukemia stages
Similar to acute lymphocytic leukemia, acute myeloid leukemia (AML) doesn’t have a standard staging system. Instead, HCPs may generally refer to the cancer as:
- AML in remission: There are no signs of AML following treatment.
- Refractory AML: Newly diagnosed AML has not responded to chemotherapy.
- Relapsed (recurrent) AML: ALL has returned after being in remission.
- Untreated AML: AML is newly diagnosed and has not been treated.
Another classification system for AML is from the World Health Organization (WHO), which categorizes AML according to factors that can affect a person’s prognosis. These classifications include:
- AML with certain genetic abnormalities: AML that displays specific types of genetic or chromosomal mutations (chromosomes are thread-like structures in cells that contain DNA)
- AML with myelodysplasia-related changes: AML with mutations associated with myelodysplastic syndromes
- AML related to previous chemotherapy or radiation therapy
- AML not otherwise specified: This refers to AML that doesn’t necessarily fit into the above categories.
- Myeloid sarcoma: AML that produces a rare tumor (called a chloroma) in soft tissues, rather than in the bone marrow
- Myeloid proliferations related to Down Syndrome
Chronic myeloid leukemia stages
Chronic myeloid leukemia (CML) is classified into three main phases instead of stages. These phases include the:
- Chronic phase: Blast cells (a type of immature acute leukemia cell) make up less than 10 percent of blood and bone marrow samples, and symptoms are mild or absent. Most people are diagnosed during the chronic phase of CML.
- Accelerated phase: CML is more advanced than in the chronic phase, with blast cells making up 10 to 19 percent of bone marrow. Noticeable symptoms such as unintended weight loss, reduced appetite, and fever may occur.
- Blast phase: Blast cells make up at least 20 percent of blood and bone marrow samples. Blasts are present in large clusters in the bone marrow, and cancer has traveled to distant parts of the body.
How is leukemia treated?

The goal of leukemia treatment is to achieve complete remission, meaning there aren’t any detectable signs or symptoms of leukemia. People who stay in remission for a certain number of years are generally considered to be cured, depending on what type of leukemia they have. For instance, acute myeloid leukemia is usually considered cured after five years of complete remission without relapse.
Leukemia treatment is typically overseen by an oncologist, a medical doctor who specializes in evaluating and treating cancer. Your care team will also likely include other HCPs, such as a hematologist (a doctor who specializes in blood disorders).
Your best course of leukemia treatment will be tailored to your diagnosis, symptoms, other health conditions you may have, and care preferences. In general, though, most leukemia treatment plans involve a combination of the following methods:
Chemotherapy (chemo): Chemotherapy is the primary form of treatment for leukemia. It uses potent, anti-cancer drugs to attack rapidly dividing cells throughout the body. Chemo may involve one drug or a combination of drugs, and it may be given as a pill, shot, or an injection into a vein.
Radiation therapy: Radiation therapy uses high-energy beams or X-rays to damage leukemia cells or slow their growth in a specific area. A machine called a linear accelerator is used to direct radiation to precise points in the body. In other cases, radiation therapy may be administered throughout the body to prepare for a bone marrow transplant.
Bone marrow transplantation: Also known as a stem cell transplant, a bone marrow transplant replaces cancerous cells destroyed by chemo or radiation therapy with healthy blood-forming cells to help restore the bone marrow. These healthy cells may come from a donor (in a process called an allogenic transplant), or they may be taken from your own bone marrow (an autologous transplant) before you receive treatment. Bone marrow transplantation can help boost the number of healthy cells in the body and regulate blood cell counts.
Immunotherapy: Immunotherapy (also called biologic therapy) uses the body’s own immune system to seek out and target leukemia cells. Ordinarily, cancer cells produce proteins that enable them to essentially hide from the immune system. Immunotherapy works by disrupting this process, allowing the immune system to view cancer as a threat and respond by generating more immune cells.
Chimeric antigen receptor T-cell (CAR T) therapy: Considered a form of immunotherapy, CAR T therapy involves genetically modifying the patient’s own immune cells to better target their cancer. Treatment involves taking a sample of the patient’s blood, separating infection-fighting white blood cells called T-cells from other blood components, and injecting the T-cells with an inactive virus that communicates new genetic instructions. The modified T-cells are then infused back into the patient, having been prepared to target and destroy leukemia cells.
Targeted therapy: A relatively new form of leukemia treatment, targeted therapy disrupts the inner workings of a cancer cell to damage it or prevent it from multiplying. For example, a targeted therapy drug may focus on a specific gene or protein of a cell to cut off its blood supply or directly eliminate it. Different types of targeted therapy drugs (such as tyrosine kinase inhibitors, also known as TKIs, and monoclonal antibodies) are used to address different types of leukemia cells.
Clinical trials: Clinical trials are research studies that involve humans. Many clinical trials are currently underway with the goal of improving outcomes for people with leukemia, though there are risks involved in participating since the therapies are often new and unproven. To learn if you’re eligible for a clinical trial, speak with your HCP. You can also access the National Cancer Institute (NCI) website to find leukemia clinical trials supported or sponsored by the NCI.
What are the possible complications of leukemia?
Leukemia disrupts healthy blood cell production in the bone marrow, which can lead to a wide range of complications. The most common include:
- Anemia: A lack of healthy red blood cells in the body can cause symptoms like fatigue, headaches, rapid heartbeat, chest pain, dizziness, and shortness of breath.
- Thrombocytopenia: A lack of healthy blood platelets can cause heavy bleeding, potentially in the digestive tract or brain.
- Serious infections: A lack of healthy white blood cells weakens the immune system’s response to germs and increases the risk of frequent or severe infections. A seemingly minor cold, urinary tract infection, or skin infection could progress to a life-threatening health concern like sepsis. Sepsis is an intense reaction by the body to an infection. In its most severe form, it can lead to tissue damage, organ failure, and death.
Superior vena cava syndrome (SVCS) is a possible complication of leukemia that spreads to the brain or spinal cord. In SVCS, the superior vena cava (an important blood vessel that returns blood from the upper body to the heart) becomes blocked, causing symptoms like shortness of breath, cough, and swelling in the face, neck, arms, or hands.
Potential side effects of leukemia treatment
Receiving treatment for leukemia also comes with some risk of complications. Because chemo can impact healthy cells as well as leukemia cells, it’s common to experience side effects like nausea, vomiting, or hair loss. Complications such as deep vein thrombosis (a blood clot in a vein deep in the body), neutropenia (a lack of healthy white blood cells), and trouble concentrating or remembering things (known as “chemo brain”) may also occur.
Another possible complication of leukemia treatment is graft versus host disease (GVHD). This can occur after a bone marrow transplant in which donor cells were used. In GVHD, the newly transplanted donor cells recognize the patient’s body as foreign and launch an immune response against healthy tissues. Symptoms can occur as late as two years after the transplant procedure and may involve abdominal pain, skin rashes, nausea, vomiting, and diarrhea.
If you experience possible signs of complications from leukemia or its treatment, contact your HCP right away.
When should you see a healthcare provider?

You should speak with a healthcare provider (HCP) if you develop any new or unusual symptoms, even if they’re vague or seem to be related to a more common condition like a cold or flu. It’s especially important to seek medical care if your symptoms are severe or if they persist for more than a few weeks without improving.
Consulting with an HCP who can evaluate your symptoms, identify their cause, and suggest appropriate treatment is always a good idea. Like most cancers, leukemia is often easier to treat when it’s diagnosed early.
Be sure to seek immediate medical treatment if you or someone around you has received a cancer diagnosis and experiences symptoms that may require emergency medical care, such as:
- Confusion
- Trouble breathing
- Chest pain
- Chills and shaking
- Bloody urine
- An intense headache with a stiff neck
- A fever of 100.4 degrees Fahrenheit
Also, be sure to get prompt medical care from your HCP if you have leukemia and experience the following:
- Abdominal pain
- Burning or pain with urination
- Cloudy urine
- Cough
- Diarrhea
- Ear pain
- Gum or tooth pain
- Headache or severe facial or sinus pain
- Mouth sores or a white coating on your tongue or parts of your mouth
- Rash or skin sores, including sores near the anus
- Redness or swelling anywhere, including a cut or wound
- Sore or stiff neck
- Sore throat
- Vaginal itching or discharge
What questions should you ask your healthcare provider?
A leukemia diagnosis can feel overwhelming and lead to confusion and uncertainty about what to do next. Find some clarity and equip yourself to make informed decisions by asking your HCP questions about your diagnosis and treatment plan. You might find it helpful to jot down your concerns before you speak with your HCP, or you can get the conversation started by asking these basic questions:
- Can you explain my diagnosis in simple terms?
- Should I get a second or third opinion?
- Is leukemia curable? What is the main goal of treatment?
- Do I have to start leukemia treatment immediately?
- When should I seek emergency care for leukemia symptoms?
- Can I go to school or work during treatment? How will this impact my daily routine?
- What are the potential side effects of leukemia treatment?
- Am I eligible to participate in a clinical trial?
- Is there anything I can do to help improve my prognosis? What things should I avoid?
- What supportive care services should I look into?
- Can you connect me to a cancer support group, either in-person or online?
Remember, never be afraid to ask questions. Staying informed about your condition and treatment options can help you more confidently navigate life with cancer.
Can you prevent leukemia?
There’s no way to prevent leukemia—in fact, most people with the disease don’t have any controllable risk factors. Still, there are a few steps you can take to help lower your risk of blood cancer and boost your overall health. These include:
- Avoiding or quitting smoking and other tobacco products
- Maintaining a healthy body weight by staying physically active and eating a nutrient-rich diet
- Limiting your exposure to benzene and formaldehyde at work or home, if possible
What is the outlook for people with leukemia?
The NCI lists leukemia as the seventh leading cause of cancer death in the U.S., but advances in blood cancer diagnostics and treatment are helping more people achieve positive outcomes. Leukemia death rates are steadily dropping, and treatments like targeted therapies and immunotherapies are helping people live better, longer.
According to the NCI, the five-year relative survival rate (how many people are alive five years after their diagnosis) for all types of leukemia combined is 66.7 percent. (Compare that to just 35.7 percent in 1975.) The five-year relative survival rate for each type of leukemia as of 2023 is:
- 71.3 percent for acute lymphocytic leukemia
- 88 percent for chronic lymphocytic leukemia
- 31.7 percent for acute myeloid leukemia
- 70.6 percent for chronic myeloid leukemia
Leukemia death rates are highest among people between the ages of 75 and 84, with 76 being the median age at death.
It’s important to remember that no two people or cases of leukemia are the same. Several factors will influence a person’s leukemia prognosis, including age, overall health, lifestyle habits, leukemia type, stage at diagnosis, and how the cancer responds to individual treatments.
Living with leukemia

Living with leukemia presents unique challenges, but making healthy lifestyle choices and prioritizing your well-being during treatment can help you cope. Your HCP is your best source for individualized advice on how to improve your quality of life and plan for the future, but some general recommendations for people with leukemia include:
Take steps to protect your mental health
Leukemia can take its toll on your mental health as well as your physical health. According to a 2022 study published in Blood Advances, around one in five adults aged 67 and older with newly diagnosed blood cancer had precancerous or cancer-associated depression or anxiety. Findings like these indicate the need for improved mental health care among cancer patients.
A 2020 research summary published in Psychiatric Sciences found at least 30 to 35 percent of cancer patients contend with mental health conditions like depression, anxiety disorders, and stress- or trauma-related disorders throughout cancer treatment.
Leaning on loved ones during your cancer journey and being open about your fears and concerns can help you maintain your mental well-being during treatment. Many people with cancer find it beneficial to attend online or in-person cancer support groups. Connecting with others who face similar challenges is also helpful for caregivers who may feel burned out or are finding it hard to cope with the challenges of caring for a loved one with cancer.
Another way to prioritize your emotional well-being during leukemia treatment is to speak with a licensed mental health provider, such as a psychiatrist, psychologist, or a clinical social worker. These professionals can help you better manage your thoughts and navigate the difficult situations you may face during your cancer journey. Some mental health providers are specially trained to help children and teens handle the emotions of living with cancer.
Nourish your body
Good nutrition is an essential part of living well with leukemia. Nourishing your body with healthy, whole foods can support your immune system and help replenish blood cells and tissues damaged by cancer or its treatment, helping you feel stronger and more energized.
The Leukemia & Lymphoma Society (LLS) recommends maintaining a varied, nutrient-rich diet that includes plenty of:
- Vegetables and fruits
- Healthy oils, such as olive oil
- Whole grains
- Lean proteins such as poultry and low-fat meats
- Fat-free or low-fat dairy
The LLS also advises people to:
- Consume less sodium (found in salt), aiming to keep it to less than 2,300 milligrams daily or as advised by your HCP
- Limit or avoid added sugars
- Limit or avoid trans and saturated fats (found in items like butter, fried foods, and many commercial baked goods)
A wholesome diet is just one component of a healthy lifestyle. In addition to making smart dietary choices to help lower your cancer risk, it’s beneficial for people with (or without) leukemia to:
- Avoid or limit alcohol consumption.
- Quit smoking or using other tobacco products.
- Drink enough water.
- Get enough sleep (between seven and nine hours per night for adults, eight to 10 hours for teens, nine to 12 hours for school-aged children, and 10 to 13 hours for young children between ages 3 and 5).
- Relax more and practice helpful stress-management techniques such as through meditation or by doing activities that bring you joy. This can include listening to music that soothes your soul or even singing karaoke to your heart’s content.
Stay on the move
Exercising is one of the best things you can do for your brain and body if you have leukemia or any other type of cancer. Engaging in physical activity (to the best of your ability) may help:
- Improve your mood and reduce symptoms of depression and anxiety
- Decrease treatment-related fatigue
- Boost heart health and lung health
- Enhance strength, balance, and overall physical fitness
- Improve sleep
- Achieve or maintain a healthy body weight
According to the Oncology-Nutrition-Exercise (ONE) Group at Penn State College of Medicine, exercise can help improve some blood cancer-related side effects and preserve a person’s ability to tend to everyday responsibilities during treatment.
Strength training and aerobic exercises are proven to be particularly helpful for individuals with blood cancer, as these movements may encourage new blood cell production. Examples of strength-training activities include lifting light weights, working with resistance bands, and doing body weight exercises like push-ups. Simple aerobic exercises include brisk walking and cycling.
Before embarking on a new exercise routine, be sure to speak with your HCP about what type and amount of activity is appropriate for your diagnosis, symptoms, and overall health. Cancer is physically taxing, and pushing your body beyond its limits won't deliver the health-boosting benefits you’re looking for.
Combining sensible nutrition, healthy movement, and compassionate mental health care with clinical treatment from your HCP can help you live better with leukemia. For additional support following a leukemia diagnosis, reach out to your care team or browse resources from patient-focused organizations like the American Cancer Society or the Leukemia & Lymphoma Society.
Featured leukemia articles

American Cancer Society. Acute Myeloid Leukemia (AML) Subtypes and Prognostic Factors. Last revised August 21, 2018.
American Cancer Society. Key Statistics for Childhood Leukemia. Last revised January 12, 2023.
American Cancer Society. Key Statistics for Chronic Lymphocytic Leukemia. Last revised January 12, 2023.
Blood Cancer UK. Blood Cancer Symptoms. Accessed August 28, 2023.
Canadian Cancer Society. Reducing Your Risk for Leukemia. Accessed August 30, 2023.
American Society of Clinical Oncology. Exercise During Cancer Treatment. Cancer.Net. Last reviewed June 2022.
American Society of Clinical Oncology. Leukemia – Acute Myeloid – AML: Subtypes. Cancer.Net. Last reviewed April 2022.
American Society of Clinical Oncology. When to Call the Doctor During Cancer Treatment. Cancer.Net. Last reviewed August 2020.
Caruso R, Breitbart W. Mental health care in oncology. Contemporary perspective on the psychosocial burden of cancer and evidence-based interventions. Epidemiol Psychiatr Sci. 2020;29:e86.
Centers for Disease Control and Prevention. Side Effects of Cancer Treatment. Last reviewed May 15, 2023.
Chennamadhavuni A, Lyengar V, Mukkamalla SKR, et al. Leukemia. StatPearls [Internet]. Last updated January 17, 2023.
Cleveland Clinic. Acute Lymphoblastic Leukemia (ALL). Last reviewed April 25, 2023.
Cleveland Clinic. CAR T-Cell Therapy. Last reviewed January 19, 2022.
Cleveland Clinic. Leukemia. Last reviewed May 18, 2022.
Cleveland Clinic. Lymphatic System. Last reviewed July 31, 2023.
Eden RE, Coviello JM. Chronic Myelogenous Leukemia. StatPearls [Internet]. Last updated January 16, 2023.
Emadi A, Law JY. Acute Lymphoblastic Leukemia (ALL). Merck Manuals Consumer Version. Last reviewed July 2022.
Emadi A, Law JY. Acute Myeloid Leukemia (AML). Merck Manuals Consumer Version. Last reviewed July 2022.
Emadi A, Law JY. Chronic Lymphocytic Leukemia (CLL). Merck Manuals Consumer Version. Last reviewed July 2022.
Emadi A, Law JY. Chronic Myeloid Leukemia (CML). Merck Manuals Consumer Version. Last reviewed July 2022.
Emadi A, Law JY. Myelodysplastic Syndrome (MDS). Merck Manuals Consumer Version. Last reviewed July 2022.
Emadi A, Law JY. Overview of Leukemia. Merck Manuals Consumer Version. Last reviewed July 2022.
Esposito, L. What Does Remission Mean for Leukemia? U.S. News & World Report Health. Published April 22, 2020.
International Agency for Research on Cancer. Estimated Number of New Cases in 2020, World, Both Sexes, All Ages (excl. NMSC). Accessed August 28, 2023.
Iyer SG, Elias L, Stanchina M, Watts J. The treatment of acute promyelocytic leukemia in 2023: Paradigm, advances, and future directions. Front Oncol. 2023;12:1062524. Published 2023 Jan 18.
Kuczmarski TM, Jaung T, Mancuso CE, et al. Precancer and cancer-associated depression and anxiety among older adults with blood cancers in the United States. Blood Adv. 2022;6(4):1126-1136.
Leukemia & Lymphoma Society. Food and Nutrition. Accessed August 31, 2023.
Mass General Cancer Center. Learn About Myeloproliferative Neoplasms. Accessed August 29, 2023.
Mayo Clinic. Leukemia. Last reviewed September 21, 2022.
Memorial Sloan Kettering Cancer Center. Risk Factors for Leukemia. Accessed August 29, 2023.
National Cancer Institute. Acute Myeloid Leukemia Treatment (PDQ®)–Patient Version. Last updated September 8, 2023.
National Cancer Institute. Advances in Leukemia Research. Last reviewed August 1, 2023.
National Cancer Institute. Find NCI-Supported Clinical Trials. Accessed September 12, 2023.
National Cancer Institute. Leukemia—Patient Version. Accessed August 23, 2023.
National Cancer Institute. Chronic Lymphocytic Leukemia Treatment (PDQ®)–Patient Version. Last updated August 26, 2022.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Leukemia. Accessed August 23, 2023.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Leukemia–Acute Lymphocytic Leukemia. Accessed August 28, 2023.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Leukemia–Acute Myeloid Leukemia. Accessed August 28, 2023.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Leukemia – Chronic Lymphocytic Leukemia. Accessed August 28, 2023.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Leukemia–Chronic Myeloid Leukemia. Accessed August 28, 2023.
Nemours KidsHealth. Kids and Sleep. Last reviewed January 2021.
Nemours KidsHealth. What Is DNA? Accessed August 28, 2023.
Northwestern Medicine. What Are the Stages of Leukemia? Accessed August 29, 2023.
Penn Medicine. Graft Versus Host Disease (GVH). Last reviewed April 29, 2022.
Penn Medicine Abramson Cancer Center. Leukemia Diagnosis. Accessed August 29, 2023.
Penn Medicine Abramson Cancer Center. Types of Leukemia. Accessed August 24, 2023.
Penn State Health. Exercise Can Be Beneficial for People Diagnosed with Blood Cancers. Published February 1, 2022.
Stanford Medicine. Stages of Acute Lymphoblastic Leukemia. Accessed August 29, 2023.
Sausen DG, Basith A, Muqeemuddin S. EBV and lymphomagenesis. Cancers (Basel). 2023;15(7):2133.




