Updated on May 19, 2022
Surgery is one of the most common treatments for breast cancer. In recent years, surgeons have found ways to make operations safer, more successful, and less invasive. Medical advances mean people with breast cancer can now choose from different surgeries, including:
- Breast-conserving surgery, also called lumpectomy
- Mastectomy with flat closures
- Mastectomy with breast reconstruction
These options can let you build a treatment plan around your priorities and lifestyle, as well as the severity of your breast cancer diagnosis. That said, having to make an important decision at a time when you may already be emotionally or physically exhausted can feel overwhelming.
Mark Mugiishi, MD is president and CEO of the Hawaii Medical Service Association and a former surgeon specializing in breast surgery at Ekahi Health-Central Medical Clinic in Honolulu. Here, he provides straightforward answers to top questions about what each procedure entails to help you feel confident about your final decision.
Surgery to diagnose breast cancer
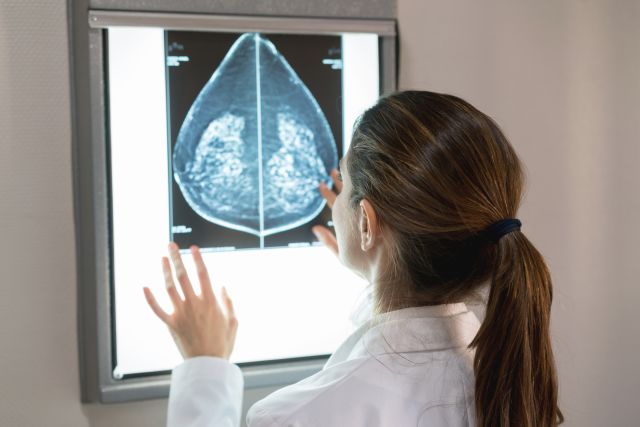
“Surgery is used to both diagnose and treat breast cancer,” says Dr. Mugiishi. If a concerning area shows up on a mammogram or an ultrasound scan, surgeons use a needle to take a sample of the spot. They will then look at it under a microscope to make a diagnosis.
This procedure, called a biopsy, is the only way your surgeon can confirm that a painful lump, a spot on your mammogram, or a change in your breast is cancer.
Surgery to remove cancer
You and your healthcare provider (HCP) may discuss a number of possible surgeries, depending on your diagnosis and personal preferences. For most people, choices include:
Breast-conserving surgery (BCS), also known as lumpectomy: The goal of BCS is to remove the tumor, plus some of the healthy tissue around it, called the margin. The margin is then tested to determine if the entire tumor has been successfully removed or if cancer cells may have been left behind. The amount of breast tissue removed depends on the size of the lump, its location, and the advancement of cancer, among other factors.
Whenever possible, surgeons try to do BCS—as long as everything around the tumor is healthy tissue—because it preserves the breast, says Mugiishi.
The recovery time for BCS is relatively short. It can be done as an outpatient procedure, meaning you won’t have to spend the night in the hospital.
“Afterwards, you’ll be able to resume activities when you see fit,” Mugiishi says, although it may take some people as long as two weeks.
Most people who undergo BCS also need radiation, a type of therapy that uses powerful rays to destroy leftover cancer cells. Radiation is a local treatment, aimed at only the part of the breast that has been affected by cancer. Every person reacts differently, but radiation may cause side effects like exhaustion and skin irritation. Radiation may also cause long-term changes to the size, coloration, pores, sensitivity, and thickness of breasts.
Mastectomy: A mastectomy involves removing the entire breast. Depending on how far the cancer has spread, some of the structures around it, like chest muscles and lymph nodes, might be taken out, too. This surgery may require a hospital stay, and it may be a few weeks before you’re back to your old routine.
You might undergo a mastectomy instead of BCS depending on certain characteristics of the tumor or conditions you have may, including:
- Your tumor is large or there’s not a clear margin around it
- You have multiple tumors
- You don’t want or can’t have radiation
- You’ve already had BCS in that breast, but the cancer came back
- You have mutations in the BRCA1 or BRCA2 gene
- You’re at high risk for a second cancer
- You have inflammatory breast cancer, a particularly aggressive form of the disease
Some pregnant people who have breast cancer may also be advised to have a mastectomy instead of BCS.
Mastectomy with reconstruction: You may choose to have breast reconstruction performed immediately after your mastectomy. This surgery will rebuild the shape of the breast after a mastectomy. (It’s also an option after a more invasive BCS procedure.)
Even if you wait a while before undergoing reconstruction, it’s still important to speak with both a surgical oncologist with a specialty in breast cancer and a plastic surgeon before your mastectomy. There are different types of breast reconstruction, so your HCP can help you decide the best approach for you.
“If you’re going to have reconstructive surgery in the future, you might even get the plastic surgeon who’s going to be involved in the initial mastectomy operation,” says Mugiishi. “They can align the scars exactly the way they would for reconstruction.”
Checking for the spread of cancer
Your surgeon will most likely perform a sentinel node biopsy during breast cancer removal surgery. Lymph nodes are tiny glands that collect waste, germs, and cancer cells, and then filter them out of the body. When cancer spreads, it tends to reach certain lymph nodes, or “sentinel nodes” first. A sentinel node biopsy involves removing the lymph node or nodes (usually one to three) that filter and drain the breast tumor area, and then checking them for cancer. The surgeon will send the biopsy to a lab so a research technician can view the cells under a microscope to confirm or rule out cancer.
“If the sentinel node doesn't have cancer in it, then there's no need to remove any more,” says Mugiishi. If cancer has reached the first lymph node, your surgeon may need to take additional nodes from your armpit area to determine how far the cancer has spread.
Survival rates, compared
In 2021, JAMA Surgery published a Swedish study of 48,986 people comparing those who underwent BCS with those who opted for mastectomy. The researchers found that the overall 5-year survival rate for those who had BCS along with radiation was higher (95.1 percent) than those who had mastectomy with radiation (86 percent). The 5-year survival rate for just breast cancer was 98.2 percent for the BCS with radiation group and 90.5 percent for the mastectomy plus radiation group.
It’s important to note that since you keep your breast with BCS, there’s a chance that cancer will come back in that area. If it does, you may need a mastectomy at that point, Mugiishi says.
Expectations after surgery
After your surgery, you may come home with drains that were inserted into your breast during the procedure. Some drains may be removed before you leave the hospital. If you do have drains (which may remain over the course of approximately 1 to 2 weeks after surgery), you’ll be unable to lift your arms or anything heavy.
Wearing zipped or buttoned shirts during this healing period is essential. Your healthcare team will offer tips on pain management, how to safely change bandages, and how to shower.
Ultimately, the choice between BCS and a mastectomy is highly personal. So is the choice to opt out of reconstruction. After two bouts of breast cancer at age 38, health journalist Catherine Guthrie chose this for herself after a double mastectomy. She penned a memoir, Flat: Reclaiming My Body From Breast Cancer, to talk about her journey and to encourage others to advocate for themselves.
Today show journalist Hoda Kotb, meanwhile, spoke on the air in May 2022 about her past breast cancer experience. In 2007, Kotb had a mastectomy and was at first unhappy with her surgical scars. She opted to have reconstruction and 15 years later, she shared a new sense of her overall appearance.
“Now I look at my scars, and I’m happy,” she says.
Choosing the surgery that’s right for you
When trying to decide on a surgery, you might feel a sense of urgency about removing the cancer as quickly as possible. But it’s important to take the time to do the following:
- Research your options. Ask your HCP for handouts on each procedure. As you read, make a list of questions for your surgeon, and then take notes while talking to them.
- Involve a surgical oncologist with a specialty in breast cancer in your care team if you can.
- Discuss your treatment plan with loved ones.
- Find out your family history, including if any loved ones have had cancer.
Whenever possible, get a second opinion, as well. This won’t insult your HCP; they’ll want you to feel secure in your final decision. Gathering as much information as possible can set your mind at ease and put you in control of your treatment plan.